Case Study: How Do Bacteria Become Resistant?
Part 1: What is MRSA?
No matter what doctors did, the baby's oxygen levels were dropping as drug resistant bacteria were eating holes in the lungs of the 7 week old. Even the most powerful antibiotics could not stop the infection. Just two days ago, Madeline had started coughing. Then Madeline's mother found her limp and blue in her crib and she was rushed to the hospital. She was diagnosed with pneumonia caused by bacteria. It was MRSA.
The methicillin resistant form of the bacterium commonly known as “staph” was first identified in the 1970's in hospitals, but it has since spread across the world, showing up in daycares and schools. The bacterium can sometimes "colonize" a person and not cause illness. The person can carry it on their bodies for years and pass them to other people or leave them on surfaces.
Madeline's parents wondered how she had contracted this dangerous bacterium. Madeline's family agreed to tests to determine if any of them were carrying the deadly bacteria or if the child contracted the bacteria from the hospital.
In the past, penicillin was used to treat Staphylococcus aureus infections, but the bacteria had become resistant to penicillin. During the 1950s, other antibiotics, like methicillin, were discovered that could treat Staphylococcus. The graph below shows the spread of antibiotic resistant infections. Separate curves are shown for infections from the hospital ("Hospital Acquired") and Community Acquired.
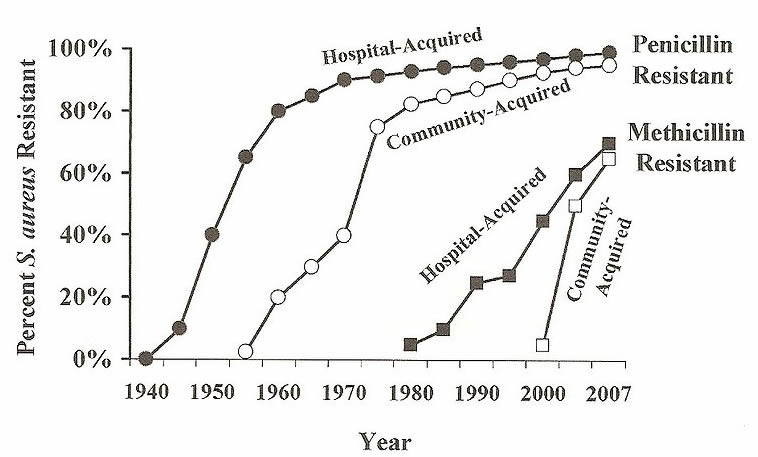
1. Based on the graph, when did 80% of hospital acquired bacteria become penicillin resistant?
When did 80% of community acquired bacteria become penicillin resistant?
2. In 2005, what percentage of hospital acquired bacteria were resistant to methicillin?
What percentage of community acquired bacteria were resistant to methicillin?
3. Based on the trends seen in the graph, what would you expect to happen to the effectiveness of methicillin to both types (community and hospital) of bacteria?
4. Propose a reason for why community acquired resistant bacteria lags behind hospital acquired:
Part 2: MRSA Screening
A methicillin resistant Staphylococcus aureus (MRSA) screen is a test that looks for the presence of MRSA. On a community level, screening may be used to help determine the source of an outbreak. Sources may include specific rooms in a hospital or school, or individuals who may be carrying the bacteria on their skin. Once a source is identified, the area can be cleaned thoroughly with antiseptics, or a person can be treated with antibiotics.
A nasal swab is collected from the nostrils of an asymptomatic person and cultured. The sample is put onto a special nutrient medium called agar. The sample is incubated in a warm area so that bacteria can grow. The sample is then examined for the growth of characteristic MRSA colonies.
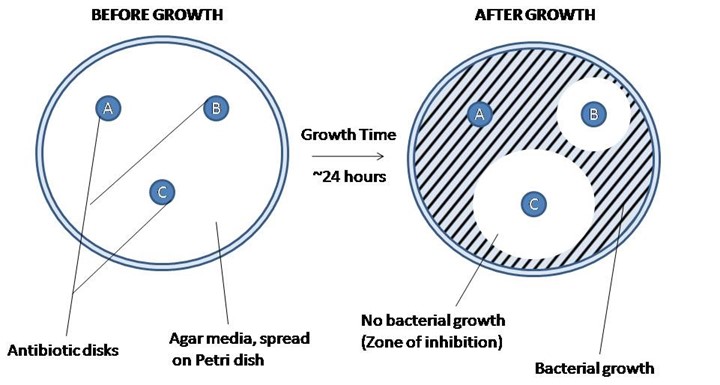
When studying how bacteria respond to antibiotics, the KirbyBauer disk method is used. In this technique, discs containing antibiotics are placed on agar where bacteria are growing, and the antibiotics diffuse out into the agar.
If an antibiotic stops the bacteria from growing, we can see circular areas around the disks where bacteria have not grown. This area is called the "zone of inhibition." The diameter of these zones is measured as shown below.
5. Bacteria are grown on what medium? ______________________
6. The area near the antibiotic disk where no bacteria grows is called the __________________________
7. Why is it important to determine the source of an outbreak? ___________________________________
8. Once the source is identified, what is the next step? __________________________________
9. What is the difference between an antibiotic and an antiseptic?
________________________________________________ ________________________________
10. Examine the image above. Which of the bacteria (A, B, or C) is resistant to the antibiotic? _______
Part 3: Analyzing the Plates
Each plate below represents a sample taken in the investigation. Nasal swabs were taken from individual family members and two samples were taken from the hospital delivery room. The samples were grown on agar with antibiotic disks added.
PE = penicillin | ME = methicillin | CE = cephalothin | VA = vancomycin
11. Measure the zones of inhibition on the plates and record the data in the table. Measure in millimeters.
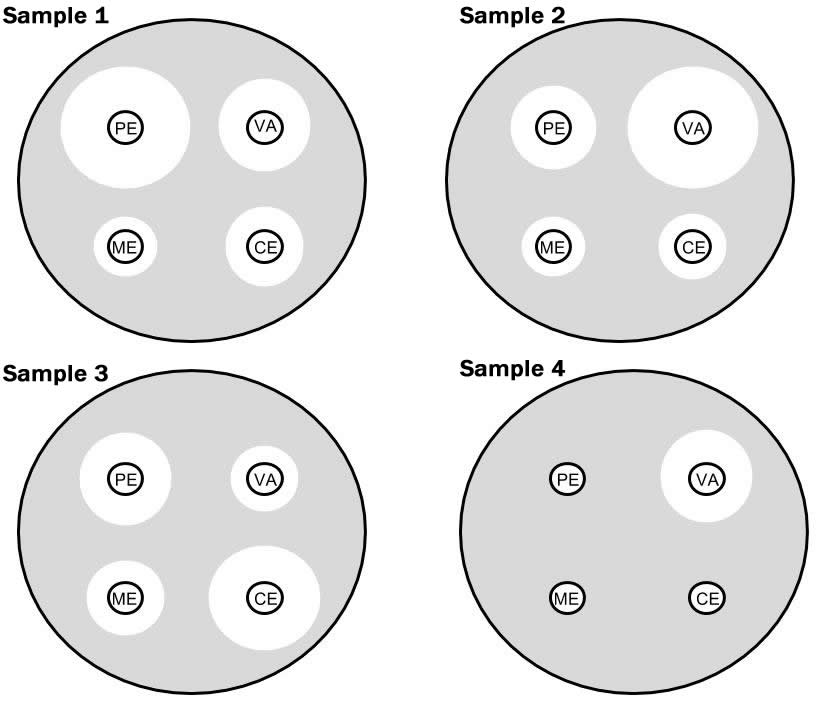
| Sample | Disk | Zone Size | Sample | Disk | Zone Size | |
| 1 | PE | 3 | PE | |||
| ME | ME | |||||
| CE | CE | |||||
| VA | VA | |||||
| 2 | PE | 4 | PE | |||
| ME | ME | |||||
| CE | CE | |||||
| VA | VA |
Part 4: Conclusions
12. The following table identifies the sample sources. Which sample contains MRSA?
| Sample 1 | Madeline's Mother | |
| Sample 2 | Madeline's Sister | |
| Sample 3 | Madeline's Father | |
| Sample 4 | Delivery Room Surface |
13. Sample 1 was taken from a nasal swab of a family member who has been having sinus infections.
What antibiotic would be most successful for treating the infection? _______________________
What antibiotic would be most successful for treating Madeline’s sister? ____________________
14. Based on the data, where did Madeline contract her infection? Explain how you know.
15. What antibiotic would be most effective for Madeline’s infection? Explain your choice.
16. What recommendations would you make to Madeline's family and the hospital where Madeline was delivered. Your recommendations should include evidence based reasoning and details from the case to support your position.
Based on this story: http://newsblogs.chicagotribune.com/triage/2009/07/a-family-battles-mrsa-after-losing-a-child.html
Resources: http://labtestsonline.org/understanding/analytes/mrsa/tab/test/
Baby Photo from Morguefile
Graph Source: http://wiki.ggc.usg.edu/wiki/Staphylococcus_Fall_%2711

